Welcome Back Rheumatology Fans,
I am trying something new this week so let me know what you think. This is a case study with some learning points. The idea is to demonstrate some of the nuance in clinic with people who turn up without text book symptom profiles.
For the avoidance of doubt - any similarities to real people are completely coincidental
Now, about half way down, you will see there is a “Clinical Reasoning Activity”. The idea is that you make some notes and see if they match up with mine. Obviously you can circumvent this by just continuing to read on… That is up to you :)
Referral
Jane (made-up) is a 35 year old female complaining of insidious onset bilateral heel pain for the last 6 weeks. She takes no regular medication. She has a past medical history of Psoriasis which is managed by moisturisers. She attended a Physiotherapist last year for repetitive strain in her hand.
Further Subjective Information
Insidious onset bilateral heel pain 6 weeks ago. She awoke one morning and was unable to weight bear through her heels. This improved after a few minutes and she ignored it. This has gradually worsened over the last 6 weeks and now she struggles to walk for the first 2 hours in the morning. No change in habits, occupation or circumstances prior to onset. Has not been unwell or required antibiotics.
She has had psoriasis for 10 years and manages this with moisturiser. Last year she developed pain and swelling in the IPJs of her index and middle finger in the right hand, this was diagnosed as a repetitive strain issue. Improved with physiotherapy and ergonomics over a few months and then resolved after 6 months.
She had Lateral Epicondylopathy 5 years ago which lasted 2 years and was quite debilitating.
24 hour pattern
Severe pain in the mornings when she gets out of bed which takes 2 hours to improve. This will return to a lesser degree during the day after sitting or after walking for longer periods. Her sleep is unaffected.
Aggravating/Easing
Her heel pain is worse after sitting / driving for any period of time. This will resolve over a period of time relative to how long she was sat, from a few minutes to a few hours.
Past Medical History
She has no known health issues other than the Psoriasis. She attended her GP for the hand symptoms last year and prior to this the tennis elbow. She does not take any prescribed medications. She denies any sexually transmitted infections and use of steroids. She feels well in herself and denies feeling anxious or depressed but feels fatigued constantly.
She has no personal or family history of iritis/uveitis or crohns/colitis. Her father has Psoriatic Arthritis. She has no nail bed changes.
Social Factors
She works at a desk as an estate agent and often drives to view houses. She enjoys walking her dog 3-4 miles a day, this is not normally an issue. She smokes 10/day and has a BMI of 32.
She has been concerned about Psoriatic Arthritis since she developed the hand symptoms but was reassured as they went away.
Clinical Reasoning Activity
From the case presentation note down the indicators that Jane could have SpA
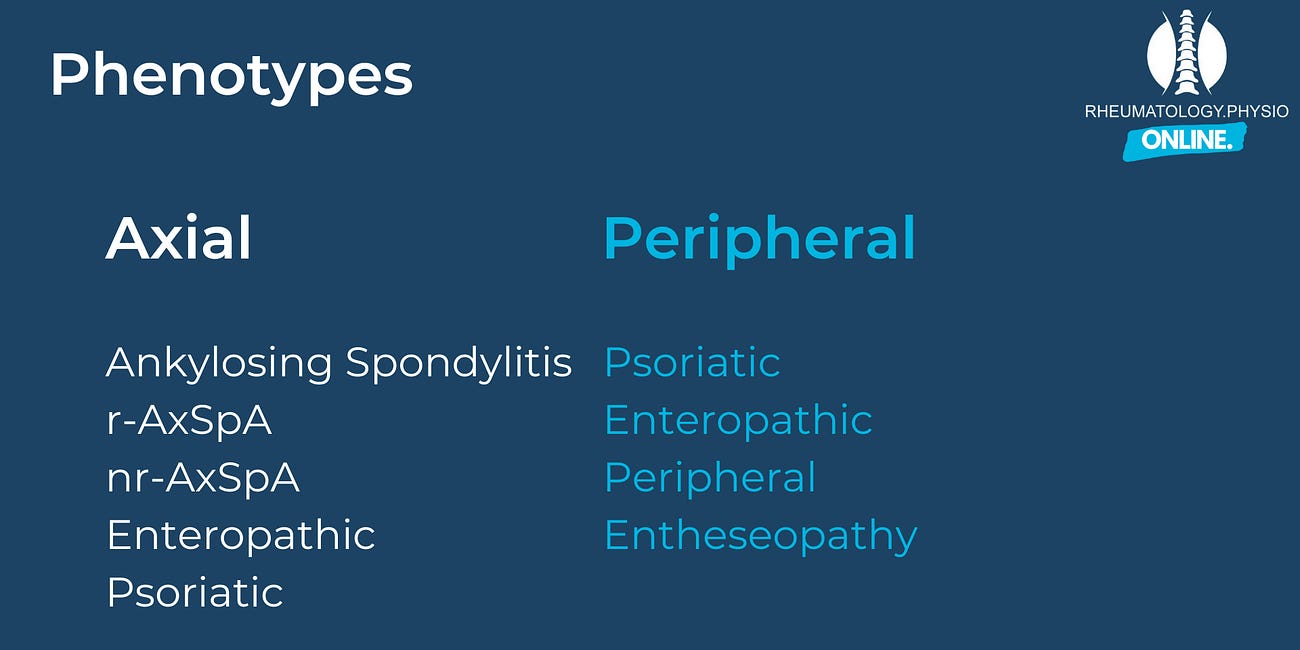
Jane is presenting with a possible Peripheral Spondyloarthritis; likely Psoriatic Arthritis.
- Insidious onset bilateral tendinopathy (plantarfasciitis)
- Symptoms in the morning for >60 mins
- Previous Lateral Epicondylopathy and previous IPJ swelling and pain
- Diagnosed Psoriasis
- Father has Psoriatic Arthritis
- High BMI and Smoker
Next Steps
Explain to Jane that the clinical picture is one suspicious of an inflammatory cause of her symptoms which needs referring to a Rheumatologist for further investigations.
The aim of this appointment is to confirm or rule out a specific diagnosis and start appropriate treatment if necessary.
Discuss with Jane her general health as her high BMI and smoking status will contribute to a raised level of systemic inflammation. This may increase the likelihood of developing Psoriatic Arthritis or the separate clinical conditions. If diagnosed with Psoriatic Arthritis, these factors will also make a poorer outcome more likely.
Consider starting specific therapy management for the bilateral heel pain to plan for the possibility Psoriatic Arthritis is ruled out.
A trial of anti-inflammatories may be worthwhile to assess impact on symptoms.
Investigations
If appropriate and available refer for:
- Ultrasound imaging to look for Insertional Enthesitis
- Blood tests: HLA-B27, ESR, CRP, Rheumatoid Factor
Onwards Referral
Refer to Rheumatology via the appropriate local pathway for further investigation of symptoms suspicious of Peripheral Spondyloarthritis (pSpA).
Learning Points
pSpA should be considered in the presence of Psoriasis and Tendinopathy even if one or both are historical
General health advice at this early stage is important accompaniment to the prompt referral for short and long term outcomes regardless of the final diagnosis
Family History of inflammatory conditions adds a strong clinical suspicion and reduces threshold for referral
In this scenario it is possible that Jane has multiple distinct clinical conditions, it is not possible to rule out pSpA and as such warrants referral for specialist investigation






Sure of course 👍
My previous article included differential diagnosis vs tendinopathy https://open.substack.com/pub/rheumatologyphysio/p/enthesitis
That part is behind the paywall though
Hi and thanks for this neat way of presenting learning material, Jack. I like it!
However, like Séamus McNally below, I too was missing the bit on differential diagnosis - I see you covered this before so I'm late to the table. Thanks for adding it.
I only say it because long ago when I first qualified, I had a patient with bilateral ankle pain, and also some intermittent dizziness. She was recently retired but had previously been an air hostess as they were then called, in times when they had to wear high hells too. She had also survived an air crash where she'd been standing serving when the plane crash-landed!
Not knowing much at about peripheral spondyloarthritis at the time, but doing a header into commission bias, I assumed these ankles must have sustained damage from the compression forces of the accident, and referred her to her doctor for this otherwise unusual presentation, and to get the dizziness checked. By the time she finally went to her GP months later, the tumour in her bowel had become so enormous as to have become inoperable. Both her bilateral ankle pain and her dizziness were put down to effects of her cancer by her specialists. Ever sine then I have followed up on such referrals promptly to make sure they have actually done what was advised.
I am no way wagging my finger here as you are such an expert, but maybe if you do continue these lovely nuggets, the DDx would be very welcome.
Many thanks again. I'll subscribe properly once my talk on Physio Matters is over! Great resource.
Helena