Being Specific With Rheumatology
Hello there Rheumatology Fans!
Introduction
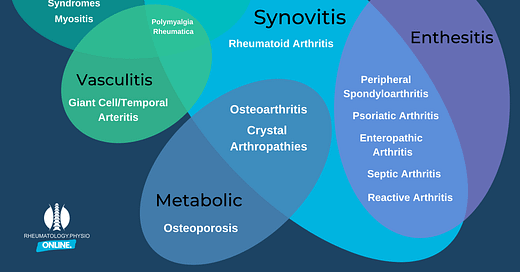
Rheumatology as a specialism that covers a hugely broad set of conditions, within each a hugely broad set of presentations whcih of course occur in individuals who bring with them their own circumstances and quirks. For MSK Therapists these Rheumatology conditions are masqueraders, conditions which look a lot like something much more common.
These are in my opinion “Red Flag” conditions while undiagnosed and need referring out of MSK to Rheumatology departments. As such I get requests for courses to upskill Therapists to recognise, investigate and refer these patients, especially in light of the increased numbers of First Contact Practitioners.
As MSK Therapists, how accurate can we be? Maybe more interestingly, how accurate should we try to be?
Complexity
Accuracy is important and I think we should be as accurate as we can be at all times for the sake of people’s understanding and journey. It also can help with pathway management, some locations have specific spinal clinics, Early Inflammatory Arthritis (EIA) clinics and Connective Tissue Disorder clinics.
This can all work against us though. Imagine a patient with bilateral hand pain, we think this is Rheumatoid Arthritis - not a terrible assumption - we run bloods and refer to an EIA clinic but the bloods come back equivocal (CRP 20, ESR 30, RF -ve), this referral is quite possibly going to be rejected. What if we were more accurate in the subjective history and we realise the person has a history of Psoriasis which we know is more likely to come back with RF -ve, a referral as suspected Psoriatic Arthritis (PsA) fits the pattern better and then maybe less likely rejected.
This is a challenge and one of the issues is there are no black and white answers. If you spend any time in a Rheumatology department this continues as an evolving picture or diagnosis over time.
It is absolutely mad to think MSK therapists would be expected to be highly accurate in these diagnoses when sometimes Consultant Rheumatologists struggle. What can we therefore do to mitigate pathway issues, yet avoid being drawn into being too specific where it is easy to miss a subtle yet important diagnostic detail.
Understand
Understanding your own limitations and the local policies is a really good place to start.
Where is your ability level with regards to understanding the relevant differences of Rheumatology diagnoses and the interplay between comorbid conditions?
This might vary between diagnoses as well, if you specialise in spines or feet you might be a lot more confident with regards to some conditions compared to others, seeing them more often or understanding the other differential diagnosis patterns more deeply
Where do you sit in the patient’s pathway?
All sorts of roles have different responsibilities, if you are working a predominantly rehabilitation role it might be that you need to recognise an inflammatory disorder and direct it to another clinician, in an APP/ESP role it may be that you are responsible for undertaking investigations, specifically referring and accessing the pathways.
What are the local pathways?
If your local Rheumatology department only has a general referral pathway, there is far less need to be specific at referral. If there are a variety of pathways (much more likely) then accessing the most appropriate one for the individual is important. Getting them to the right clinician, in the most timely manner and with appropriate workups reduces delays to diagnosis and improves experience.
What if get it wrong
We are all fallible humans, this is going to happen on occasion. I try to follow this process in Rheumatology:
Are the presenting symptoms suspicious of inflammatory pathology
Are there associated comborbidities making development of a systemic inflammatory pathology more likely
Is this most likely a Enthesitic, Synovitic or Connective Tissue problem
Can I be more specific at this time? (is it predominantly axial for example)
Which pathway or investigations would be the most appropriate given the answers to the above questions
You can always ask for help, advice or a second opinion!
Sometimes, and I have experienced this A LOT, you can be convinced about a presentation and then, by the time the person has seen someone else the symptoms have changed, new ones have come to light or they have found out a family history they didn’t know before and it changes the diagnostic outcome. You can’t do anything about this!
It’s difficult because once you have referred on you often lose the communication loop but if you do get a letter back that outlines a “misdiagnosis” (that seems far too harsh a word in this circumstance, we will get back some patients who look like they have a rheumatology disorder but actually do not) then go back over your reasoning process, see if there were any gaps, anything changed or if it was just one of those complex cases we all see from time to time.